
(1-31-18) Baltimore psychiatrist Dinah Miller, M.D., co-author of COMMITTED: The Battle Over Involuntary Psychiatric Care, has reacted to my blog about HHS Assistant Secretary Dr. McCance-Katz’s decision to put a hold on a government operated website that identifies “evidence based practices.” COMMITTED, written with her co-author Annette Hanson, M.D., recently won the Carol Davis Ethics Award given by the American Psychiatric Association each year for the best book published about ethics by psychiatrists.
Please Stop Using the term: ‘Worried Well’
Dear Pete,
Let me start by saying that after 25+ years as a psychiatrist, I’ve never heard of the NREPP website, which identifies “evidence based practices,” so I’m not certain whether closing it is a good thing or a bad thing. Instead, I’d like to respond to some of the things that were said in the course of your blog post.
You used the term “worried well.” Please don’t use that term, ever.
It implies there are people with legitimate suffering because they have “real” mental illnesses, and those whose suffering is trivial because they don’t have “serious” mental illness.
Suffering is suffering– it all hurts, and sometimes those with no obvious signs of mental illness surprise us all when something suddenly goes horribly wrong.
Psychiatric care is expensive, poorly reimbursed, time consuming, and stigmatized; people don’t present for treatment for trivial reasons.
There is the implication that some people are more deserving of care in a way we would never dream of bifurcating in any other field. Could you imagine if you went to the ER with chest pain and were derided because it turned out you had heartburn or a pulled muscle and were not having a heart attack?
As doctors, we help people who are in distress; we don’t make the distinction about whose suffering is valid and worthy of treatment.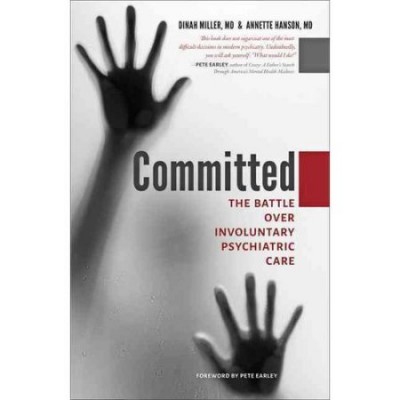
I am all in favor of giving more resources to people with chronic and disabling mental illnesses — these are society’s most disenfranchised members, their suffering and the suffering of their families is immense, and they use our resources one way or another. If not through appointments with psychiatrists and the cost of their medications, then through lost productivity, the cost for medical care incurred from unhealthy life styles, and the cost of institutionalization.
What I find difficult about these discussions is that psychiatry is the only arena where advocates ask for money for one set of patients at the expense of another. We don’t ever suggest that money to treat metastatic lung cancer should come from denying treatment to those with basal cell carcinomas.
While I have you here, I’d like to bring up a related topic that perhaps you can get the Interdepartmental Serious Mental Illness and Serious Emotional Illness Committee (a federal committee created to advise Congress) to review, one that all of us might be able to agree on.
The Real Gatekeeper To Getting Mental Health Care
When the topic turns to serious mental illness, the loudest and most controversial agenda is about legislation to make it easier to involuntarily hospitalize patients. While there are cases where this is an issue, for those of us in practice, there is a bigger issue: the real gatekeeper to getting very sick people adequate and optimal care is not the law, the gate keeper is the insurance/mangled care industry.
Insurers have a erected a barrier to inpatient treatment which has set the standard for admission as “imminent danger.”
There are times when everyone can agree that a patient needs to be in the hospital: the patient, the family, the doctor, but if that patient does not present as being dangerous, it has become nearly impossible to get him or her into a hospital bed. This has trickled into our standard of care: psychiatrists no longer try to hospitalize patients who are not dangerous (usually suicidal) because they believe an insurance company will not authorize the admission, that an ER will release the patient.
So the few available beds fill with admissions from the ER of people who are so depressed or so psychotic as to be dangerous, and elective admissions just don’t end up happening. What does happen is that the few available inpatient beds get taken by very ill, very dangerous patients and the acuity level on inpatient units is very high. They often require security officers, and the environment is anything but healing; in fact, inpatient units have a high rate of assaults for both the patients and the staff.
And then we wonder why people won’t voluntarily admit themselves to these units when they are sick.
Anosognosia: I beg to differ with the argument!
This is the point where people in favor of easier standards to involuntarily admit patients shut me down: they say the patients have anosognosia, they don’t know they are sick and they won’t get care no matter what, and issues of safe, healing environments or medications that don’t cause awful side effects are irrelevant.
I beg to differ with that argument, and still contend that if psychiatric care was kinder, better funded, more palatable, and not stigmatized, then more of those who are not aware they are ill could be swayed to get care.
Psychiatry is the only medical specialty where the standard for admission has become life-threatening illness, not just being really sick.
It would be so helpful to all of us if there were more beds available and if insurance companies were not allowed to deny admission to very sick people because there was not an imminent threat of death.
I do believe that is something that everyone in all the tents can agree on, and it’s a good starting gate for all of us.
In addition to co-authoring COMMITTED, Dr. Dinah Miller and her co-author, Annette Hanson, M.D., along with a third psychiatrist, Stephen Roy Daviss, M.D., collectively authored Shrink Rap: Three Psychiatrists Explain Their Work, Dr. Miller regularly posts her thoughts on the Shrink Rap blogpost. A psychiatrist and writer, she is in private practice and has authored four novels as well as the two non-fiction books about mental illness cited in this blog. 



