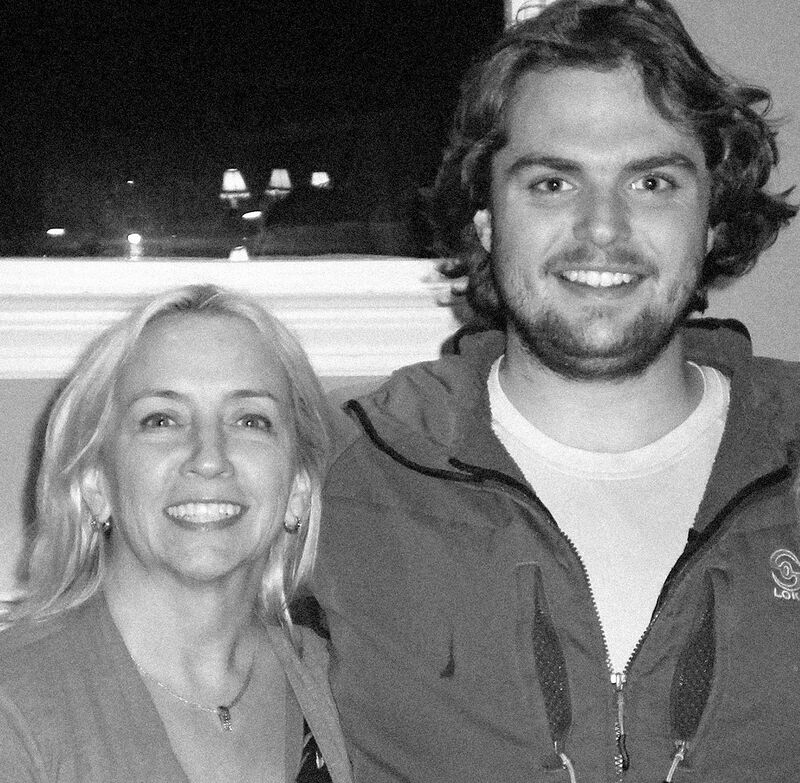
>DeeDee Tillitt and her son Max, who died of a drug overdose 10 weeks after leaving a treatment center when his insurer declined to cover a longer stay. (Courtesy of Deedee Tillitt.) From Bloomberg Businessweek.
(6-21-19) A sister describes her brother’s schizophrenia and family’s struggle, and insurance companies are getting sued for refusing mental health care to patients who then take their own lives. While I don’t typically reprint stories, these two are worth your time.
One is a reminder of how important it is to share our stories. Putting a human face on mental illnesses lessens stigma, promotes understanding. Also, please tell me on my facebook page if you have been victimized by an insurance company. I will pass your story along to former Rep. Patrick Kennedy and the appropriate members of Congress.
As Suicides Rise, Insurers Find Ways to Deny Mental Health Coverage
Red tape and a lack of in-network providers frustrate those seeking treatment.
The U.S. is in the midst of a mental health crisis. In 2017, 47,000 Americans died by suicide and 70,000 from drug overdoses. And 17.3 million adults suffered at least one major depressive episode. The Mental Health Parity and Addiction Equity Act, a landmark law passed more than a decade ago, requires insurers to provide comparable coverage for mental health and medical treatments.
Even so, insurers are denying claims, limiting coverage, and finding other ways to avoid complying with the law.
Americans are taking to the courts to address what they see as an intrinsic unfairness. DeeDee Tillitt joined one lawsuit in 2016, months after she lost her son Max. He’d been an inpatient for three weeks at a treatment center to recover from a heroin addiction and seemed to be making progress. His addiction specialist wanted him to stay. United Behavioral Health, a unit of UnitedHealth Group, the nation’s largest insurer, declined to cover a longer stay for Max. Reluctantly, his family brought him home. Ten weeks later, Max was dead of an overdose. He was 21.
My Brother Tom’s Schizophrenia
By Marin Sardy writing in The New Yorker.
My brother Tom’s slide into homelessness occurred in stages.
We never knew exactly when or how he lost his apartment, or came to crash on friends’ couches, or began having run-ins with the cops. Nor did we mark the beginning of his habit of walking incessantly, roaming the streets and bike paths of Anchorage, Alaska, our home town, as he would for the rest of his life.
Friends and family members told me, much later, that he had been spending whole days driving around the city, marking up a map with notes and arrows, pursuing a delusion about women whom he believed had been kidnapped. Once, wandering and mumbling, he was picked up by police and later told a doctor that he had been fleeing the sensation that he was “about to hear the sound of a woman scream.” Another time, when our father wasn’t home, he apparently jimmied the lock with a credit card and grabbed an old checkbook for a closed account. Then he used it to book a room at a quaint little inn downtown and to make various other purchases: collectors’ coins, geodes, a framed painting, a Persian rug, and heart-shaped pendants for some secret or imagined love.
If you Google “How to convince someone with schizophrenia to get treatment,” you discover a vast network of distraught families grappling for answers.
When met with resistance by a person in the grip of psychosis, experts advise, try to work around rigid beliefs rather than attempting to dismantle them. Don’t argue with delusions, and don’t focus on points of contention. Listen respectfully and empathize. On the message boards at Schizophrenia.com, people weigh the merits and dangers of coercion, even its harshest forms. A man with schizophrenia expresses gratitude that his parents never kicked him out when he refused treatment, saying that he would not have got better without their unwavering support. Another states that, if he hadn’t been kicked out, he would never have sought help. Although research suggests that the gentler, subtler forms of pressure may be more effective, it seems that nothing works for everybody and everything works for somebody.

Marin Sardy’s memoir, “The Edge of Every Day: Sketches of Schizophrenia,” is available on Amazon.



