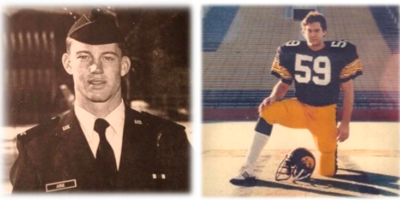
Steve Judge, left, while a cadet in the Air Force Academy, and his brother John, while playing football for the Iowa Hawkeyes. Both died because of mental illnesses. Photo courtesy of Michael Judge.
(3-15-22) This is the second part of journalist Michael Judge’s interview with Dr. E. Fuller Torrey, once named as the most influential psychiatrist in America. Part one was posted yesterday. Used with permission from Michael Judge.
The Man Who Helped Millions, Including My Family, ‘Survive Schizophrenia’
A conversation with Dr. E. Fuller Torrey, author of “Surviving Schizophrenia: A Family Manual.” He’s a rare find in today’s medical world—a psychiatrist who refuses to give up on the most severely ill.
 |
By Michael Judge (This article first appeared on The First Person With Michael Judge)
Michael Judge: My two brothers were very, very severely ill . . . one of them, John, died at 21, right before his 22nd birthday; and the other died at the age of 54.
Fuller Torrey: It’s a hard life.
It’s a hard life. So then you completed medical school and went on to become a psychiatrist. How soon after that did you publish Surviving Schizophrenia?
I went to medical school, then interned for a year in San Francisco, and then went into the Peace Corps for two years as a Peace Corps doctor in Ethiopia. Then I came back and took my residency in psychiatry at Stanford and started working on Surviving Schizophrenia, I’d say in the mid-1970s. I was in Washington with the National Institute of Mental Health (NIMH). At the same time, I took a job at St. Elizabeth’s Hospital working with the most severely ill, and found that as I was educating the families, I was saying the same things to all the families. I soon realized that I should write it down because all the families needed the information. So it was after I went to work at St. Elizabeth’s in 1976 that I started putting Surviving Schizophrenia together.
So were you doing direct, hands-on clinical work and then taking notes for the book? You came to believe you could help families that way?
Yes. I was just a regular ward doctor at St. Elizabeth’s and I had severely ill patients. And you learn very quickly when you’re taking care of them all, and also the families always wanted to know what was going on and how to help them. So that provided me with all the material. And still, when I go back and look at Surviving Schizophrenia, I remember a lot of my patients that I used as examples.
And back then, the drugs were far less helpful, right? Back then it was just a lot of Lithium and perhaps Haldol or Prolixin?
Yeah, the drugs were not as good. We didn’t have Clozapine. Clozapine came in later. But still, if you used them right, they could help a lot of patients.
Yes, my brother Steve was eventually put on Clozapine, and that was a real lifesaver for him. He went from being basically unresponsive to almost all medications and then, in the early 1990s, he got on one of the first drug trials for Clozapine, and he responded immediately. It was almost as if he had come back from the dead, you know?
Not everyone responds to Clozapine, but if they do, it can be very dramatic as you’re describing. Sadly, it’s underutilized. Even today, it’s not being prescribed nearly as often as it should be.
And part of that’s because of the high cost of doing regular blood tests—is that right—that people on Clozapine are required to take in the U.S.?
Yes, that’s one of the reasons, definitely the main reason why it’s not used as much as it should be.
Your book Surviving Schizophrenia has helped millions of families, including my own. It’s definitely changed the way the world thinks about schizophrenia. In 1998, you founded the Treatment Advocacy Center. What was the motivation behind that?
The problem with the mentally ill homeless was something I became aware of in the 1980s. I was volunteering at the shelters, the women’s shelters for homeless women in Washington, D.C. I did that for about 16 years, and I became very, very concerned about our failure to treat people with severe mental illnesses in the communities where they lived. That failure of treatment was resulting in a lot of tragedies. So I became aware of the homeless mentally ill and also the mentally ill in jails and prisons, which was becoming a real problem at that time.
And so, in 1998, after I published Nowhere to Go: The Tragic Odyssey of the Homeless Mentally Ill, and, in 1996, Out of the Shadows: Confronting America’s Mental Illness Crisis, Vada Stanley from the Stanley Medical Research Institute called me and said, “Is there anything we can do for the severely mentally ill while we wait for better treatments?” The Stanley family had already donated many millions to research. But she wanted to know specifically what we could do to help the most severely ill while we waited for the research to kick in. “Yes, I think there is,” I said. “We can start by changing state laws and making it easier to treat people.” And that was the beginning of the Treatment Advocacy Center. TAC was founded to provide help—especially to the homeless mentally ill, mentally ill in jails and prisons—while we’re waiting to find better treatments.

Dr. E. Fuller Torrey, founder Treatment Advocacy Center
A lot of these failures began a long time ago with what at first was a good idea—deinstitutionalization—but resulted in millions of untreated people in the community ending up in jails and prisons, correct?
We don’t like to blame the people who started the program, because it was a good idea. But the failure really goes right back to the 1960s and the belief that you could put people with severe mental illness in the community and they would just come and ask for help, and then you could help them. But many of them don’t ask for help because they don’t know they’re sick. They have a brain disease that does not allow them to think clearly about what they need. And so we ended up with an increasing number of people who were homeless, who were ending up in jails and prisons. It’s a problem to this day. The Treatment Advocacy Center has done a good job of trying to help, but it’s still a very big problem.
Yes. I believe TAC research shows that in 44 states a jail or prison holds more mentally ill individuals than the largest state psychiatric hospital, and people with psychiatric diseases like schizophrenia and bipolar disorder are 10 times more likely to be in a U.S. jail or prison than a hospital bed. It’s not really “deinstitutionalization” if we’re just re-institutionalizing them in prisons.
That’s right. It’s really trans-institutionalization. We’ve just transferred them from state hospitals into jails and prisons and that’s not much of an improvement.
“If you’re sitting in a university and not having to deal with the issue of real people on the streets and in jails and prison, it’s easy to say, ‘Well, you should not treat people involuntarily.’ But when you actually see what’s happening out there, and you realize how sad and dangerous it is for people with severe mental illnesses living on the streets, especially women, you feel compelled to help them survive their very, very hard lives .”
And that’s where Assisted Outpatient Treatment comes in, right? The Treatment Advocacy Center was founded to promote AOT, which are basically state laws that make treatment mandatory for some of the severest cases. You’ve talked a bit about lobbying for those laws, but why are they so important? Why are they central to your mission at TAC?
The issue is when you can treat people involuntarily. Many people who are homeless and on the streets—they don’t know they’re sick. Should we just leave them there, or can you treat them? And I have argued that leaving them on the streets to fend for themselves is very cruel. And I’ve seen the consequences of this in volunteering at the shelters. And it just seemed wrong to not provide people with treatment who need treatment. To address that we needed to change laws to make it possible to treat people, especially the most severely ill who don’t know they’re sick, involuntarily.
That’s stirred up protests on personal liberty grounds, right? You’ve been attacked on both flanks—from libertarians on the right, as well as those on the left who say you can’t do this to people. Could you talk a little bit about your struggle to educate people about this?
Yeah. If you’re sitting in a university and not having to deal with the issue of real people on the streets and in jails and prison, it’s easy to say, “Well, you should not treat people involuntarily.” But when you actually see what’s happening out there, and you realize how sad and dangerous it is for people with severe mental illnesses living on the streets, especially women, you feel compelled to help them survive their very, very hard lives. And yes, we’ve been attacked. I’ve been attacked personally since I started doing this. And I understand people are well-meaning, but they don’t have the experience. They don’t realize what’s going on.
One of the things I suggested a long time ago was that everyone at NIMH should be given a half-day a week of free time to volunteer with the seriously mentally ill on the streets, in the shelters. And if everyone at NIMH was actually seeing people who were seriously mentally ill, we’d have much better laws. We’d have much better research, and it’d be very different for those suffering the most. But the majority of people who are making the decisions, certainly in Washington, have no real experience with what they’re talking about.
Nevertheless, TAC has made progress, and now dozens of states have changed their commitment standards and have adopted AOT practices.
Yes. That’s been a big help, and it’s saved a lot of lives. And it’s not used as widely as it should be, but it’s a major accomplishment of the Treatment Advocacy Center. And in the last administration, SAMHSA has used some federal funding to increase the number of AOT programs in the country. That’s been a big help also. So yeah, we’ve definitely made progress. There’s a lot of people being treated today that would not be treated in the past. But there’s still a long way to go.
Looking back, how do you feel about the progress that’s been made since your sister was first diagnosed with schizophrenia?
I’m optimistic about the progress. I look back on what I tried to do and I’m pleased with it. There’s just so much more to do. But I’m not discouraged because I think we have a much better understanding of brain diseases in general. We have potentially better drugs, drugs like Clozapine, which we didn’t have before. So we know what to do; we’re just not doing it very well. But I’m not discouraged.
Finally, I was unaware until recently that you wrote this book in 2017, Evolving Brains, Emerging Gods: Early Humans and the Origins of Religion. Can you tell me a little about that and how it came to be?
I was a religion major in college. And so I’ve been interested in religious belief for many years, and became increasingly interested in the evolution of the brain and then linking the evolution of the brain to our concepts of God and where these concepts come from, and when they come from in terms of human evolution, when we started thinking about these things. And so that’s why I put the book together. It’s certainly the most difficult book I’ve written. But I was intrigued by what we know about the brain now, to link it to the evolution of thinking about God and where it comes from. So that’s the kind of thing I do just for fun, maybe.
When you look at someone who’s suffering terribly from severe mental illness, in what we think of as a kind of Bedlam, does that make you question the existence of God?
Well, yes. I think that’s true. I think to see what’s going on in the world and what people are experiencing, it’s hard to believe that there is a God.
Well, I want to tell you that you’ve given me faith in humanity and hope for the future. And you gave me that hope and that faith back when I was 16 years old. So thank you.
Thank you very much, Michael.
Thank you, Fuller. I’ll say hello to my mother for you.
Please do.
(The views expressed in guest blogs are those of the guest author.)
About the author:



