(8-5-22) This is the second in a three part series about books that have crossed my desk this summer written about serious mental illnesses. Author Gail McPeake, RN., uses her personal journey with her adult son, Tom, who’d been diagnosed with schizophrenia, to warn others about the risk of suicide after someone is discharged from a hospital.
Excerpt from Home Safe: The High Risk of Suicide after Hospitalization for Mental Illness by Gail McPeake, RN. (reprinted by permission.)
I lived an hour away and I had planned on picking Tom up when he was discharged, but they put him in a cab and sent him home. The next day on the phone Tom was talking erratically again, and in the evening, I saw via his home Ring security camera that he was outside his house, walking on the driveway swinging his sword.
He had a collector’s sword that he kept in his bedroom “for protection” to feel safe, but he never took it outside. Tom went back in the house, and I called him, telling him to put his sword in the safety case and lock it, which he did.
The hospital had assessed that Tom was well enough to be sent home, but within two days we realized that he needed to go back to the hospital, so my husband, Steve, and I drove to see Tom.
His house was in shambles, water bottles strewn about, tobacco on the floor of every room. Tom was pacing, pacing, talking very irrationally. He had put a six-inch knife on his belt “for protection” he said. I went in another room and called the county Access crisis team, reporting that Tom needed to go back to the hospital. They said they would come, and they arrived about a half hour later with three police officers, two case workers, and an ambulance. They talked to Tom and convinced him that he needed to go back to the hospital to “stabilize your medications.”
Tom went quietly; he was never violent or disrespectful to anyone.
Tom was taken via ambulance back to the same hospital and was readmitted, just three days after being discharged. He stayed 16 more days and had six more medication changes. Medication changes during second admission in March: Discontinued: Aripiprazole New antipsychotics started: Olanzapine (Zyprexa) (suicide ideation warning), Paliperidone (Invega) injection (suicide ideation warning) Paliperidone (suicide ideation warning) Sedative: Lorazepam (Ativan) High Blood Pressure: Lopressor -dose quadrupled Norvasc- dose doubled Mood Stabilizer: Trileptal -unchanged.
End of excerpt
Why I wrote this book.
My son was discharged from an almost month-long psychiatric hospitalization in March 2020. Two days after being discharged, he ended his life. He was 38. We were never included in the discharge planning of his many hospitalizations for psychotic breaks and never informed of this increased risk for self-harm.
How can this happen to someone in the United States after more than a half century of research and medication development for the treatment of mental illness?“
In the month after patients leave inpatient psychiatric care, their suicide death rate is 300 times higher (in the first week) and 200 times higher (in the first month) than the general population’s.” The National Action Alliance for Suicide Prevention 2019
Thousands of families are consumed with anxiety about the welfare of their loved ones with mental illness every day. Even when they are hospitalized, we must be vigilant and advocate for care. We need to be informed of this risk and included in the discharge assessment and planning so our loved ones stay safe when they return home.
- Improve family-patient contact in behavioral health units to enhance the experience and improve communication with the treatment team.
- Include family members in the discharge planning and evaluation of their loved one prior to discharge, not just by asking them if they think the person is better, but with concrete, scientific rating scales.
- Inform families of the especially high-risk period after hospital discharge and help them make a monitoring plan with the support of in-person community case management.
- Increase the options for extended care for the seriously mental ill who need more time to stabilize on new medications.
- Ensure that resources spent on community mental health include transition teams who visit within two days of discharge to assist the person and their families.
About the author: Gail McPeake is a registered nurse who spent two decades maneuvering through the mental healthcare system as case manager and advocate for her son, only to end up grieving his loss to suicide. After two years of searching for answers, Gail decided to write Home Safe as a cautionary tale for families and healthcare providers in hopes of preventing the same tragedy in others’ lives.
Gail recently retired from a long career in nursing in the field of developmental disabilities but continues to teach medication administration classes. She grew up on her parents’ grape farm in Geneva, Ohio with her eight siblings and lives with her husband in Richfield, Ohio. Gail can be contacted at remeika.mcpeake@gmail.com.

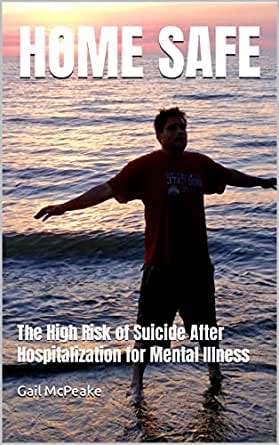
Gail and her son, Tom, in happier times. (Photo courtesy of Gail McPeake.)



