(4-12-21) Involuntary Commitment is a topic that stirs strong opinions and feelings. I asked Dinah Miller, a Baltimore, Maryland, psychiatrist, and co-author of Committed: The Battle Over Involuntary Psychiatric Care to react to last week’s blog written by Cheryl Nimtz.
What I Discovered When I Investigated Involuntary Care
By Dr. Dinah Miller.
“But, if I had not had the good fortune of being involuntarily committed and put on one tiny pill, I would still be homeless begging on the streets, in prison with little or no treatment, caught in human trafficking, swallowed by drug addiction or dead.” ~Cheryl Nimtz on Pete Earley’s Blog
It is nice to have Cheryl Nimtz come forward to share her stories, a story of how psychiatrists have helped her.
For 12 years, I wrote a blog with Drs. Anne Hanson and Steve Daviss called Shrink Rap that we began after publishing our book by the same name. We would write, and when the topic turned to forced or involuntary treatment, the comments invariably got very heated.
There was so much about the horrors of involuntary care, and it was through blogging that I discovered how psychiatry’s efforts on behalf of people with episodes of severe mental illness can be traumatizing.
We would hear from people like Cheryl too — people whose lives were chaotic, who were in imminent danger, who had been hallucinating, delusional, or remarkably disorganized and who presented a danger to themselves or others, who were then hospitalized and got better.
Assumed People Were Grateful
I just assumed people appreciated the care they received and how much better it made them. It was not until I started a blog that I discovered how injured and violated many people feel after being treated against their will, at a time when their judgment was so clouded by illness that I imagined no one would want to be left in this condition. My interest in this distress led me to co-author: Committed: The Battle Over Involuntary Psychiatric Care. 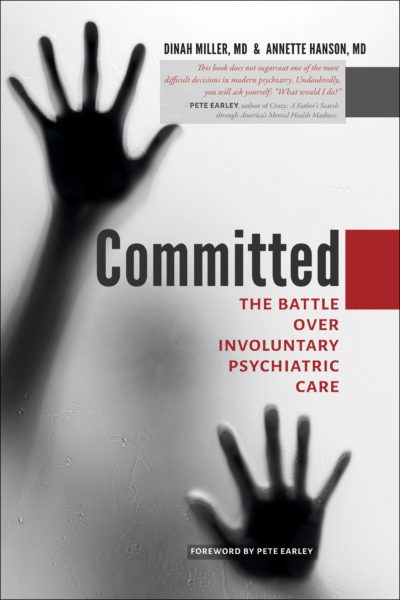
Like so many issues in our society today, the battle over involuntary psychiatric disorders is a polarized one: You’re for or against, and there’s not a lot of room for shades of gray. When we wrote the book, I knew this was going to be a book that no one would like– we didn’t choose a side and on polarized topics, people go to the extremes.
Yet, I turned out to not be a big fan of involuntary treatment if there is any way to avoid it. It is odd to me that we make so much noise in this country about getting people treated against their will when there are so many people who want what we have to offer, but can’t access care.
I think we need to put more effort into making voluntary care more accessible so that people get treatment before they get very ill. There are times, however, when there really is no choice, and it’s better to have a traumatized patient than a dead one.
I believe there should be protections of patients’ rights; our history as a field has been ugly. When it’s too easy to force people to get care, we run the risk of becoming lazy — why bother working to gain a patient’s trust if you can force them to get help? This does not endear me to those on either side of the divide. And to those who believe that the treatments we have to offer are either ineffective or harmful — I see a different world, one where people get better and live more fulfilling lives, and when people come willingly, they are appreciative and it’s so nice to be part of their journey to wellness.
Drawing A Who’s Who Diagram
When I lecture about the battle over involuntary psychiatric care, I like to present a picture of the battlefield as I see it. My battlefield is orange, because I like orange, and I fill it in with the groups on each side.
On the side of the field that is in favor of making it easier to involuntarily treat people is the Treatment Advocacy Center (TAC) and traditionally NAMI. In my depiction, NAMI is in a cloud because the group has an identity problem and I’m going to refer you back to Pete’s post on how NAMI struggles with whether they are a “big tent” advocating for everyone with psychiatric disorders or a “small tent” maintaining the interests of those with serious mental disorders:
I might contend that the small tent is populated not by those with serious disorders, but by their parents and by some psychiatrists — those who want to see them get well. The American Psychiatric Association (APA) almost didn’t make it to my battlefield: psychiatrists as a group don’t have a unified stand. I placed APA on the chart just to the left of the center because in 2015 the APA came out with a very carefully worded statement in favor of outpatient commitment under very specific circumstances.
The groups that are opposed to legislation that will make involuntary treatment easier to access are: the Recovery Movement — a group founded by consumers who advocate for their autonomy; the Bazelon Center for Mental Health Law; Mad in America; MindFreedom International, founded by David Oaks, a psychiatric “survivor;” and the Citizens Commission on Human Rights (CCHR) founded by psychiatrist Thomas Szasz together with the Church of Scientology.
What Does My Chart Tell You?
Do you notice something?
Those on the “pro” side of my orange battlefield are generally the devastated parents of those with psychiatric disorders who are helplessly watching their children struggle, who want a better life for them and feel that if only they could be forced to get care, then they would live better, safer, and healthier lives. The others on that side of the battlefield are psychiatrists.
The opposition groups consist mostly of people who feel they have been injured by psychiatry and civil rights attorneys.
What’s missing?
I will tell you: there are no organized groups of patients shouting out about how involuntary care helped them and how it should be easier for others to get this care!
This brings me back to Cheryl Nimtz and her remarkable voice saying that involuntary treatment was a good thing. In our polarized world, it is not easy to find people who have been helped and are shouting from the rooftops. It is so nice to hear that someone who was suffering so much is doing so well!
About The Author: Dr. Dinah Miller is a psychiatrist in Baltimore, Maryland. She received her medical degree from Weill Cornell Medical College of Cornell University and has been in practice for more than 20 years.




