An investigative report recently released by the Inspector General’s Office in the Virginia Behavioral Health and Developmental Services Department is causing a stir. Each year, the IG is required to make unannounced visits to state facilities that treat persons with mental disorders and report his findings. 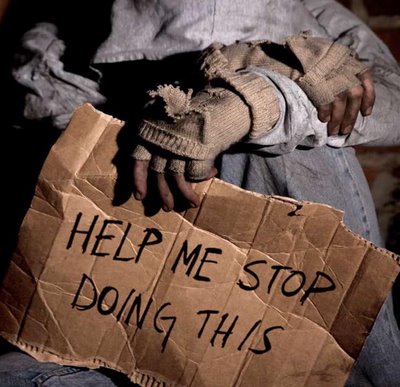
The section of G. Douglas Bevelacqua’s report that is getting the most attention, especially from the National Alliance on Mental Illness Virginia Chapter is the IG’s discovery that “streeting” is now a common practice in Virginia. “Streeting” is the term that hospitals use when someone, who should be admitted, is turned out onto the street because there are no beds available. (More on this in a future blog.)
It’s another discovery that Bevelacqua cites that I want to discuss here.
In his report, Bevelacqua writes that a federal regulation is being so narrowly interpreted by Virginia Attorney General Kenneth T. Cuccinelli that as many as ten percent of patients in state run facilities are being denied access to treatment that could help them recover.
Patients are being denied “medically necessary interventions that would allow them to participate in their treatment.” They are being “denied palliative care” and their rights to helpful treatment are being “restricted,” the IG claims.
Kenneth T. Cuccinelli is well-known in Virginia mental health circles. When he was running for office, he talked about his efforts as a state legislator to improve mental health services. I spoke to him about the need to reform Virginia’s mental health system and he was well versed in the problems that our state faces. He sees himself as a friend of persons with mental illnesses.
So why is the IG suggesting that Cuccinelli’s office and a federal rule – that was written to protect persons with mental illnesses from abuse –are actually causing great harm to patients in Virginia?
Here is how this dust up started.
On March 15, 2011, the Inspector General received a complaint from a court appointed guardian who said that doctors at a Virginia facility were refusing to inject a patient with an antipsychotic medication that, in the past, had been effective in treating the patient’s severe mental illness. The guardian feared that, without this drug, the patient would sink “further into a psychotic state.” Withholding the drug was going to “prolong psychosis that could cause permanent damage” to the point that “the patient might never return to his/her previous level of function,” the guardian warned.
The IG immediately dispatched investigators to the hospital to look into the guardian’s charges. When they got there, they discovered that the patient’s psychiatrist and the patient’s treatment team agreed with the guardian. They strongly recommended that the patient be given an injection of a long acting anti-psychotic medication. Otherwise, the health of the patient would be seriously threatened. (The report does not say whether the patient is a male or female. I have chosen to use the traditionally ‘he’ for clarity.)
In addition to speaking to hospital officials, the IG investigators interviewed the patient. When they asked him why he didn’t want to get the injection, the patient explained that he didn’t want the shot because the doctors at the hospital were not really physicians. They were secret government agents and the drug would cause him to divulge national security secrets.
It was at this point that the Attorney General’s office entered the picture. Hospital officials said they would have to restrain the patient first in order to give him the shot. While it might only take a few minutes, there was no way to give him the shot without using restraints.
The hospital had been told by Cuccinelli’s office that if they restrained the patient, even for a few minutes, they would be violating 42 CFR Part 482, a federal rule that governs the use of restraints. Cuccinelli’s office said the regulation forbids the use of restraints for any reason except when there is an emergency that involves “immediate physical safety.” (Dangerousness.)
Here is what the rule states:
All patients have the right to be free from physical or mental abuse, and corporal punishment. All patients have the right to be free from restraint or seclusion, of any form, imposed as a means of coercion, discipline, convenience, or retaliation by staff. Restraint or seclusion may only be imposed to ensure the immediate physical safety of the patient, a staff member or others and must be discontinued at the earliest possible time.”
Continuing the rule states:
Often with the best intentions, a patient or the patient’s family may ask for a restraint to be applied….A request from a patient or family member for the application of a restraint which they would consider to be beneficial is not a sufficient basis for the use of a restraint intervention. Regardless of whether restraint use is voluntary or involuntary, if restraint is used, then the requirement of the regulation must be met. (immediate physical safety)
The IG wrote: “In other words, regardless of an individual’s capacity to make informed decisions about their medical care, a nonviolent psychotic patient can only be medicated if he/she agrees to the injection, and a delusional person, lacking the capacity to make informed decisions, can only be restrained to be medicated once the immediate physical safety to self or others threshold has been crossed. A seriously mentally ill person, lacking capacity, who poses no immediate danger to his/her physical safety cannot be medicated — unless they agree to treatment.”
The IG wrote that Cuccinelli’s interpretation of the rule stopped the guardian and hospital from giving the injection. The IG then said that even if a patient wrote in an advance directive, when he was thinking clearly, that it was okay for hospital officials to restraint him if he became psychotic in order to give him medication, hospital officials could not legally do it unless he was threatening the physical safety of others.
Bevelacqua has sent a letter to the administrator for the Centers for Medicare and Medicaid Service in the Department of Health and Human Services asking him to clarify the rule. In that letter, Bevelacqua poses this question:
Can a patient, who is capable of making an informed decision, put a clause in his advance directive stating that he wants a hospital to use restraints and give him antipsychotic drugs if he becomes ill — regardless of whether or not he is dangerous?
In his report, the IG wrote: “It is ironic that an interpretation of a Federal regulation whose stated purpose is to ‘insure each patient’s physical and emotional health and safety’ disenfranchises scores of psychotic, but nonviolent, patients in Virginia’s behavioral health facilities who are denied medically necessary interventions that would allow them to participate in their own lives.”
The reason why I find this interesting is because it deals with the same issue that kept me from getting my son help when he was psychotic. When should doctors be permitted to step in and help someone with medication if they lack the capacity to make a rational decision. Under Cuccinelli’s interpretation of the restraint rule, it doesn’t matter if doctors, legal guardians appointed by the court, or even the patient himself (through an advance directive) wants medication. Unless that patient becomes threatening and poses an “immediate physical safety” threat, nothing can be done.
What’s your view? And if you believe the “immediate physical safety” theshold is too high for restraints, what should it be?
Who is right here — the IG or AG or neither of them?




Clearly, he should have been able to get the shot.
As a parent who witnessed my son being restrained on more than one occasion, I can attest that restraints should only be used for physical safety. BUT, I’m a bit confused here. It seems that there are two distinct issues here; the threshold for when a person should be medicated, and another for when restraints should be used. I’m assuming it would have been legal to give the patient medication against his will if they had been able to do it without restraints, because, as stated, the “patient’s treatment team …strongly recommended that the patient be given an injection of a long acting anti-psychotic medication. Otherwise, the health of the patient would be seriously threatened”. I agree that immediate physical safety should not be the only reason for medication. So, if that decision was legal, and the staff is stating that the only way to give medication is by restraining the patient briefly, it must be because they or the patient’s physical safety would be in jeopardy while administering what is right and legal for the patient. If that is the case, they are within the limits of the law regarding restraints as well. Is the AG the only one who doesn’t understand this distinction? Or am I missing something? Allowing another human being to remain in a prolonged psychotic state when there is an alternative, is both unbelievably cruel and tragically all too common. While I also believe that only medication, without ongoing treatment availability is just as cruel, that’s an argument for another day.
Attorney General Kenneth Cuccinelli send me this response this morning after he read what I had posted on my blog.
Dear Pete,
I think the answer is to get the reg changed-its too restrictive, but proper (ie effective) language could be tricky to come up with. If you know of existing language somewhere that addresses this issue, I’d be happy to take it to the feds to try to get it implemented.
Dear Pete,
A third option for patients suffering from psychosis is to test for and treat medical conditions and substances that are known to induce psychosis. It not only saves money, but saves lives.
If a doctor can rule out this list of possible causes, then they should be allowed to “step in and help someone with medication”.
Medical conditions which can induce psychosis include: brain tumors, cerebrovascular disease, Huntington’s disease, multiple sclerosis, Creitzfeld-Jakob disease, anti-NMDAR Encephalitis, herpes zoster-associated encephalitis, head trauma, infections such as neurosyphilis, epilepsy, auditory or visual nerve injury or impairment, deafness, migraine, endocrine disturbances, metabolic disturbances, vitamin B12 deficiency, a decrease in blood gases such as oxygen or carbon dioxide or imbalances in blood sugar levels, and autoimmune disorders with central nervous system involvement such as systemic lupus erythematosus have also been known to cause psychosis.
A substance-induced psychotic disorder, by definition, is directly caused by the effects of drugs including alcohol, medications, and toxins. Psychotic symptoms can result from intoxication on alcohol, amphetamines (and related substances), cannabis (marijuana), cocaine, hallucinogens, inhalants, opioids, phencyclidine (PCP) and related substances, sedatives, hypnotics, anxiolytics, and other or unknown substances. Psychotic symptoms can also result from withdrawal from alcohol, sedatives, hypnotics, anxiolytics, and other or unknown substances.
Some medications that may induce psychotic symptoms include anesthetics and analgesics, anticholinergic agents, anticonvulsants, antihistamines, antihypertensive and cardiovascular medications, antimicrobial medications, antiparkinsonian medications, chemotherapeutic agents, corticosteroids, gastrointestinal medications, muscle relaxants, nonsteroidal anti-inflammatory medications, other over-the-counter medications, antidepressant medications, and disulfiram . Toxins that may induce psychotic symptoms include anticholinesterase, organophosphate insecticides, nerve gases, heavy metals, carbon monoxide, carbon dioxide, and volatile substances (such as fuel or paint).
Do you realize all psychiatric medications have harmful side effects?
Do you realize there are psychiatrists using accupuncture, Integrative Psychiatry, Orthomolecular Psychiatry, and Functional Medicine with successful outcomes?
Do you realize Diedra Sanbourne may have died from a bowel obstruction caused by Clozapine?
Do you care?
I can assure you this is the last comment I will post on your site, as this is the last post of yours I will waste my time reading.
Deafness doesn’t cause psychosis. And my mother has had MS for 30 years and I’ve never seen it make her psychotic.
The “harmful” side effects of “all” psychiatric meds is no more harmful than side effects from any prescribed meds and they help you live a better life than the one you live without them. Clearly you have never been in a psychotic episode so bad that you didnt know reality from fiction.
I don’t agree with your statement. Psych med side effects are much more severe than most other prescription meds. I’ve taken just about all of them. Antipsychotics, for example, on average shorten the lifespan due to severe cardiovascular harm and massive weight gain. It may be that the side effects are worth it, for some patients, but don’t whitewash the horrible side effect profile of antipsychotics. If the drugs are helping only a little bit, they are not worth the risks. If you are psychotic and the pills are a magic bullet, then they may be worth it.
Brilliant blog. I am not a lawyer. Thinking this through, I am a little unclear: I thought a guardian could make decisions in the client’s stead…that a decision by a guardian was the same as a decision by the client. If that’s the case, since the client could request the treatment and could request being constrained if needed, I don’t quite understand why an issue arose. On the bigger picture, it seems to me that we should be moving to a “lack of capacity’ standard rather than relying on ‘dangerousness’. Anyone courts say (and it should be courts) can not make their own decision, should have someone doing it for them…like we do with alzheimers and minors. The surrogate decisionmaker could decide not to treat, to treat or something in between. But if someone can’t make their own decisions, it doesn’t make sense to say ‘so be it. We’ll wait till your dangerous. What do you think?
There is a solution that Cucinnelli isn’t pointing out, but it requires a specific court order in the absence of an emergency. A general order giving a guardian power to make medication decisions won’t cut it, and raises all kinds of constitutional questions in this context that a specific order does not. The safest thing for any guardian in that situation is to go back to the court anyway. Unfortunately, this is expensive. Even more unfortunately, it puts everyone in the position of letting the patient deteriorate until the issue can be addressed the a judge.
DHS has addressed this issue in its interpretive guidelines to its regulations.
The advanced publication from the federal Department of Human Services dated April 11, 2008 Ref. S&C-08-18 states at p. 94, , “A court order for medication treatment only removes the patient’s right to refuse medication. Additionally in accordance with State law, some patients may be medicated against their will in certain emergency circumstances. However, in both of these circumstances, health care staff is expected to use the least restrictive method of administering the medication to avoid or reduce the use of force, when possible. The use of force in order to medicate a patient, as with other restraint, must have a physician’s order prior to the application of the restraint (use of force). If physical holding for forced medication is necessary with a violent patient, the 1-hour face-to-face evaluation requirement would also apply.”
So what is needed is 1)a court order and 2)use of force only when it is really, really necessary. In some states thes are constitutional requirements, anyway.
Commitment, AOT and guardianship laws can be written so that the initial commitment/AOT court order incorporates a finding, based on evidence from the patient and clinicians, that the mentally ill patient is in need of medication, and, due to the patient’s illness, is incapable of making a rational treatment decision. The court then orders medication subject to defined appeal rights, time limits, etc. In other words, the order doesn’t last for ever–it can and should be revisited when circumstances change. Questions like the one posted above about whether the patient really needs antipsychotic medications as opposed to something else should be addressed
in the court hearing(s) where the patient will be represented by an advocate. Assuming the court orders medication, it is then up to the clinicians to find the best way to administer the medication, using as little “force” as possible (which is only common sense). The one option they don’t have is disobeying a direct court order.
All rights of patients, because of physical or mental conflict and punishment. Rights of all patients not to be intimidated.
athletic supplement
In 2008, I saw a woman in the psych unit who had dementia tackled by 8 people, dragged off to the seclusion room, where she was stripped naked and left to sit on the floor while a staff person watched her one to one. Many male patients said they were allowed to walk by that room and saw her sitting on the floor naked. Her offense? She ripped up a sheet of paper and threw the bits of paper on the floor. she deteriorated dramatically during her inpatient stay at a Catholic community hospital that has a good reputation.
I have seen many other abuses.
when I reported this information (and other abuses) to the hospital accreditation agency, all they cared about was if the electric razors were sanitized after patient use.
I will say that the hospital took my complaints seriously, and changes were made. But I took careful notes and spent many hours polishing my complaint letter, and worked with the state’s ombudmsan, also.
The entire mental health system is systematically re-traumatizing patients who already commonly led lives of hell as children or young adults. At a state hospital, nurses taunted a man who had PTSD from his honorable service in the army. I was restrained for at least 6 hours, and nobody checked on me that entire time. I could have been dead there in the restraints, and they wouldn’t have known. I should have peed myself and let them deal with that.
I think the law is fine the way it is, and I am glad I know about the new law. I will have to make mention of it in my advance directive, which I already spent a hundred hours working on that thing, to protect myself from the abuse of burn out staff. (most staff have always been nice, the abusers do it when the nice people are not around).
Recommended long-acting injections of antipsychotic drugs patients receive. Who government agents and drugs that you disclose national security secrets.
Protective Table Pads