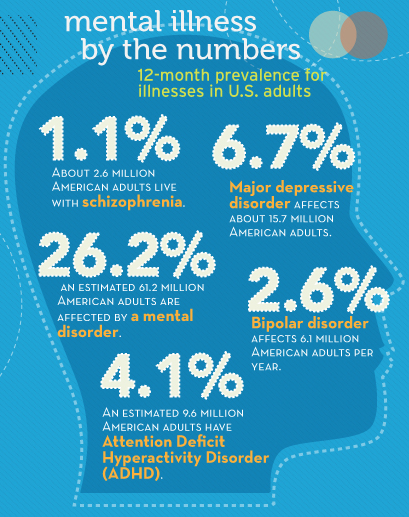
FROM MY FILES FRIDAY: A year ago, I published this letter from a young woman dealing with her’s father’s mental illness and her own. I hope you find it as compelling as I did and still do.
Hi Pete Earley,
…I came across your book while looking for a source of comfort during my own family’s time of need. Two months ago, my dad was finally forced into treatment for his undiagnosed severe bipolar disorder and coexisting extreme alcoholism. My mother and I (I am an only child) have been trying unsuccessfully for years to get him help.
In order for him to finally be involuntary subjected to treatment, he had to have a major traumatic psychotic episode and had to contact Help 4 Addiction for his alcohol rehabilitation. He had a previous psychotic episode earlier this year that landed him in a mental health facility for one week. But the latest one proved even more traumatic to all of us.

 I turned sixty-two last Thursday and my wife, Patti, hosted a family party on Sunday. When you have a blended family of seven, there’s always someone having a birthday but this one was different for me. I can’t say that I am going through a mid-life crisis because I already have done that, several times. I am now old enough to collect Social Security so I have to acknowledge that I have walked over the middle age line .
I turned sixty-two last Thursday and my wife, Patti, hosted a family party on Sunday. When you have a blended family of seven, there’s always someone having a birthday but this one was different for me. I can’t say that I am going through a mid-life crisis because I already have done that, several times. I am now old enough to collect Social Security so I have to acknowledge that I have walked over the middle age line .