Nick Maher at sentencing hearing.
(9-22-22) Should someone with a severe mental illness be blamed for “choosing” to be ill if they refuse treatment and later become violent?
A prosecutor in Genesee County, New York, argued earlier this month that Nicholas Maher, age 38, deserved a maximum prison sentence because he’d refused to take medication and seek treatment prior to him fatally stabbing his 69 year-old father, Martin Maher, last year.
“Nick Maher is a college-educated person,” District Attorney Kevin Finnell told a judge. “He’s smart enough to know that he needs to get mental health treatment and that he needs to take his medication, even if it doesn’t make him feel real good. But he chose not to do that.” Finnell said Maher was clearly responsible for his father’s death, even though the prosecution and defense agreed that Maher was legally insane when he attacked his father.
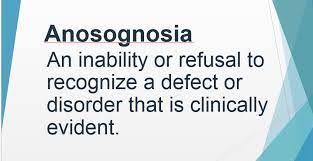
Maher had no prior criminal history, but he had a long history of mental illness, his defense attorney, Public Defender Jerry Ader told the court. “I sincerely believe that our community, our country, has a difficult time dealing with mental illness, especially when it comes to mental illness in the criminal justice system.” Ader questioned whether Maher had enough insight to “choose to be ill.”
“Some (said) he chose to do these things, and that he could have done something else. And I’m just not quite sure that’s true. And I don’t think anyone can know for sure if that’s true. It’s easy to say because we don’t understand mental illness. But in my experience, when someone is placed in a psychiatric hospital, it could take years in order to get a patient, an inmate, to understand, to have the insight as to their illness, why they need help and why they need medication.”