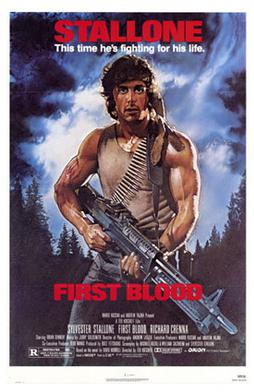
Theatrical release poster by Drew Struzan taken from Wikipedia
(7-6-20) I received a slew of emails about last week’s blog that called for shifting responsibility of the seriously mentally ill from the police to social service agencies and the medical community.
One long-time reader chastised me for unintentionally spreading a “cheap stereotype” of American soldiers when I wrote:
“No one wants RAMBO answering a mental health call.”
In a separate email, Virgil Stucker, who became president emeritus of the CooperRiis Healing Community in 2017 after serving as founding Executive Director from 2003, took issue with this statement:
“We have never shut down longer term treatment facilities. We simply have made them only available to individuals who can afford the high costs of such excellent facilities as McLean Hospital or such healing communities as Gould Farm or CooperRiis.”
Here’s what both had to say:
Dear Mr. Earley,
I’ve been an avid follow of your blog for quite some time now. Today I read your post: Defunding the Police and Serious Mental Illness: Opportunities, Hard Questions, Dangers. In the section entitled “Training Will Not Fix The Problem,” I read a line that bothered me quite a bit. You wrote “No one wants RAMBO answering a mental health call.” This single sentence has several problems.
To begin, I think you need to go watch First Blood, the movie that introduced cinema-goers to the character of John Rambo. In this film Rambo is a homeless veteran, depicted as suffering from what seems to be PTSD-like symptoms. He is walking across the country seeking out friends that he served with. The movie does end up becoming an 80’s action-fest, but only after Rambo is harassed, arrested, and brutalized by the local sheriff’s department. Rambo is not my enemy, he is me. Like me, he is a tortured soul suffering from mental illness. When his liberty is abused by local law enforcement he snaps and falls back on his special forces training. I am not trained as such, but I absolutely dread the idea of having an encounter with hostile law enforcement officers.
 Washington D.C. area. She is the station’s health reporter and played a pivotal role in developing NBC Channel 4’s long-running educational news series about mental illness called
Washington D.C. area. She is the station’s health reporter and played a pivotal role in developing NBC Channel 4’s long-running educational news series about mental illness called