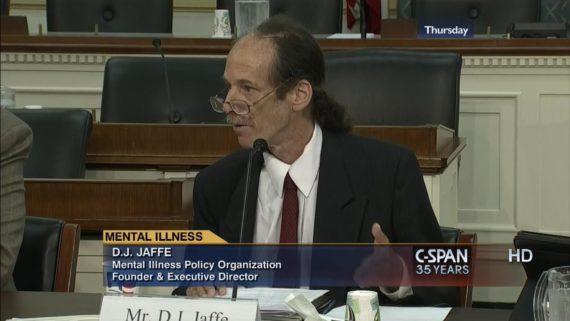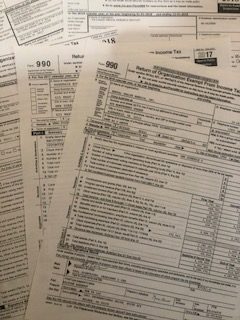
(12-16-19) All of us receive requests at year end from mental health organizations seeking much needed charitable donations. Before writing a check, I always find it helpful to examine each charity’s IRS Form 990, which is available on the Guidestar website.
I check three numbers: the amount of revenues that were received, the amount of net assets that the organization lists at year end, and how much a nonprofit group pays its CEO. Mental health groups must be competitive so it is not surprising that most CEO salaries are in the same $200,000 range here in Washington D.C.. That is higher than the national average. CEOs who manage organizations with multimillion dollar budgets are generally better compensated.
A quick Internet check found this thumbnail guideline:
An operating budget of a nonprofit organization under $500,000 corresponded with a CEO salary of $60,206. The highest category matched an operating budget of $50,000,000 with a CEO salary of $317,024. The average nonprofit CEO makes a little more than $120,000 a year, according to the 2016 Charity CEO Compensation Study by Charity Navigator.
Of course, there is other useful information on the tax forms. Forms reported in this blog are from the latest available reports on Guidestar.
So how do mental health nonprofits compare?