(4-12-19) What a nice surprise!
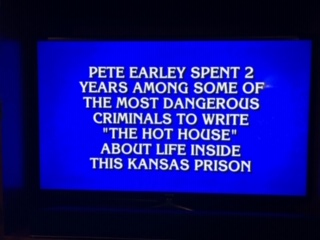
The screenshot shows a clue from the popular television game show Jeopardy.
The correct answer under the category of true crime books was “Leavenworth,” although host, Alex Trebek, let the contestant off easy by not asking which prison. I did my research inside the U.S. Penitentiary, one of five major prisons in that community.
The Hot House: Life Inside Leavenworth Prison, was first published in 1992 but it continues to be my best-selling book.Click to continue…