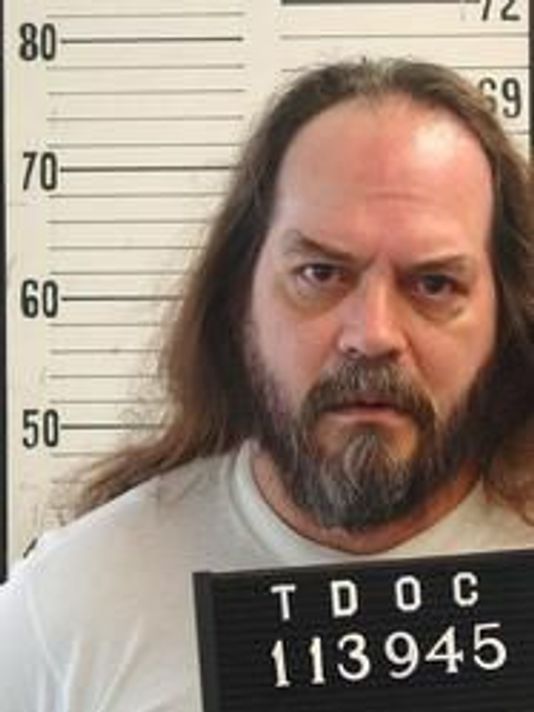
(Andrew Nelles/The Tennessean via AP)
(8-10-18) Pleas by the National Alliance on Mental Illness national office and NAMI’s Tennessee chapter to stop the execution of a seriously mentally ill inmate failed last night. Billy Ray Irick, who was convicted in 1986 of raping and murdering a 7-year old girl during a psychotic break, was administered a lethal dose of toxic chemicals in Nashville. He was 59 and had been on death row 32 years.
NAMI had asked its members to petition Gov. Bill Haslam to commute Irick’s sentence to life in prison without parole. The governor demurred, saying his role was “not to be the 13th juror or the judge or to impose (his) personal views but to carefully review the judicial process to make sure it was full and fair.”
In a statement seeking commutation, NAMI argued that information about Irick’s mental illness was never properly considered during his trial and sentencing.
Ironically, last minute appeals to the U.S. Supreme Court to stop Irick’s death hinged, not on his mental condition (witnesses testified he had the mental acuity of a seven to nine year old) but whether the lethal drugs used to execute him were appropriate.
Arguably, his case is an example of the difficulty our justice system has in determining whether a crime was committed because of a person’s impaired thinking or because of their criminality. As I wrote earlier this week, there were repeated warning signs that Irick was both mentally ill and violent. Yet, no one intervened, even hours before the murder when he was seen muttering to himself in a half-drunk rage. Court records show Irick heard voices and was “taking instructions from the devil” before he was left alone to babysit Paula Dyer. This was after family members observed him chasing a young girl in Knoxville with a machete.